Introduction
Step 1 - Preparation
Step 1.1 - Tray preparation
Step 1.2 - Patient preparation
Step 1.3 - Operator preparation
Step 2 - Place electrodes
Step 2.1 - Place the limb electrodes
Step 2.1.1 - Bipolar limb leads
Step 2.1.2 - Unipolar limb leads: augmented leads
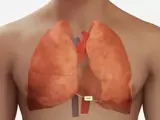
Step 2.2 - Place the chest electrodes
Step 2.2.1 - Unipolar leads: Chest leads
Step 3 - Record the ECG
Step 3.1 - Enter the patient's details into the machine
Step 3.2 - Check the machine is calibrated
Step 3.3 - Record the ECG
Step 3.4 - Annotate the presence of symptoms on the ECG tracing
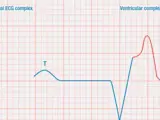
Step 4 - Analyze the rhythm strip (2 lead)
Step 4.1 - Assess the rate
Step 4.1.1 - The 6-second ECG count
Step 4.1.2 - Count large squares
Step 4.1.3 - Count small squares
Step 4.1.4 - Sequence method
Step 4.2 - Assess the rhythm
Step 4.2.1 - Ventricular rhythm
Step 4.2.2 - Atrial rhythm
Step 4.2.3 - Regularity
Step 4.3 - Identify and assess the P wave
Step 4.4 - Assess the intervals (conduction)
Step 4.4.1 - PR interval
Step 4.4.2 - QRS duration
Step 4.4.3 - QT interval
Step 4.5 - Evaluate overall appearance
Step 5 - Sinus rhythms
Step 5.1 - Features of sinus rhythms
Step 5.2 - Sinus bradycardia
Step 5.3 - Sinus tachycardia
Step 5.4 - Sinus arrhythmia
Step 5.5 - Sinoatrial block
Step 5.6 - Sinus arrest
Step 6 - Atrial arrhythmia
Step 6.1 - Premature atrial complexes (PACs)
Step 6.2 - Wandering atrial pacemaker
Step 6.3 - Multifocal atrial tachycardia
Step 6.4 - Supraventricular tachycardia
Step 6.4.1 - Atrial tachycardia
Step 6.4.2 - AVNRT
Step 6.4.3 - AVRT
Step 6.5 - Atrial flutter
Step 6.6 - Atrial fibrillation
Step 7 - Junctional arrhythmia
Step 7.1 - Premature junctional complexes (PJCs)
Step 7.2 - Junctional escape beats/rhythm
Step 7.3 - Accelerated junctional rhythm
Step 7.4 - Junctional tachycardia
Step 8 - Ventricular arrhythmia
Step 8.1 - Premature ventricular complexes
Step 8.1.1 - Types of PVC
Step 8.2 - Ventricular escape beats
Step 8.3 - Idioventricular rhythm
Step 8.4 - Accelerated idioventricular rhythm (AIVR)
Step 8.5 - Ventricular tachycardia (VT)
Step 8.5.1 - Types of VT
Step 8.6 - Ventricular fibrillation (VF)
Step 8.7 - Asystole
Step 8.8 - Pulseless electrical activity
Step 9 - AV blocks
Step 9.1 - First-degree AV block
Step 9.2 - Second-degree AV block
Step 9.2.1 - Second-degree AV block type I (Wenckebach, or Mobitz type I)
Step 9.2.2 - Second-degree AV block type II (Mobitz type II)
Step 9.2.3 - Second-degree AV block, 2:1 conduction (2:1 AV block)
Step 9.3 - Third-degree/complete AV block
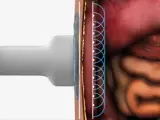
Step 10 - Pacemaker rhythms
Step 10.1 - Pacemaker terminology
Step 10.2 - Pacemaker systems
Step 10.2.1 - Single-chamber pacemakers
Step 10.2.2 - Dual-chamber pacemakers
Step 10.2.3 - Transcutaneous pacing
Step 10.3 - Pacemaker malfunction and complications
Step 10.4 - Analyzing pacemaker function with an ECG
Step 11 - Interpret the 12-lead ECG
Step 11.1 - Normal 12-lead ECG
Step 11.1.1 - Leads
Step 11.1.2 - Layout of the 12-lead ECG
Step 11.2 - Axis
Step 11.2.1 - Vectors
Step 11.2.2 - Einthoven's triangle/Hexaxial reference system
Step 11.2.3 - Two-lead method of axis determination
Step 11.3 - Myocardial ischemia
Step 11.3.1 - ST segment changes
Step 11.3.2 - T wave changes
Step 11.4 - Myocardial infarction
Step 11.4.1 - ST changes
Step 11.4.2 - T wave changes
Step 11.4.3 - Q waves
Step 11.5 - Pericarditis
Step 11.6 - Pericardial effusion
Step 11.7 - Electrolyte imbalance
Step 11.7.1 - Imbalance of sodium ions
Step 11.7.2 - Imbalance of calcium ions
Step 11.7.3 - Imbalance of magnesium ions
Step 11.7.4 - Imbalance of potassium ions
Step 11.8 - Conduction abnormalities
Step 11.8.1 - Right bundle branch block
Step 11.8.2 - Left bundle branch block
Step 11.9 - Analyzing an ECG
Step 11.9.1 - Systematic method
Step 12 - Stress testing and Holter monitoring